Hap Prior Authorization Form
Hap Prior Authorization Form - Emergency room visits don’t require prior authorization. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. For inpatient hospital stays, your doctor will get prior authorization from hap. Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable.
Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. For inpatient hospital stays, your doctor will get prior authorization from hap. Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. Emergency room visits don’t require prior authorization.
Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. For inpatient hospital stays, your doctor will get prior authorization from hap. Emergency room visits don’t require prior authorization. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health.
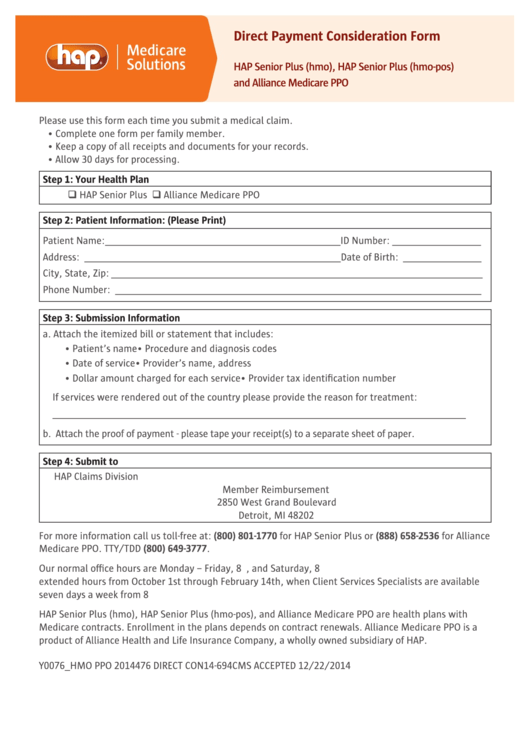
Hap Direct Payment Consideration Form printable pdf download
Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Emergency room visits don’t require prior authorization. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned.
Fillable Online Prior Authorization Criteria Form Fax Email Print
Emergency room visits don’t require prior authorization. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness.
Efficient Ways to Handle Prior Authorization Process
Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Emergency room visits don’t require prior authorization. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness.
Fillable Online Hap Prior Authorization Form PDF Fill Out and Sign
Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Participating physicians.
Investment Thesis Reports — FCA Venture Partners
Emergency room visits don’t require prior authorization. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and.
Fillable Online MIMEDP2339255 MI HAP Fillable Pharmacy Prior
Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations. Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Emergency room.
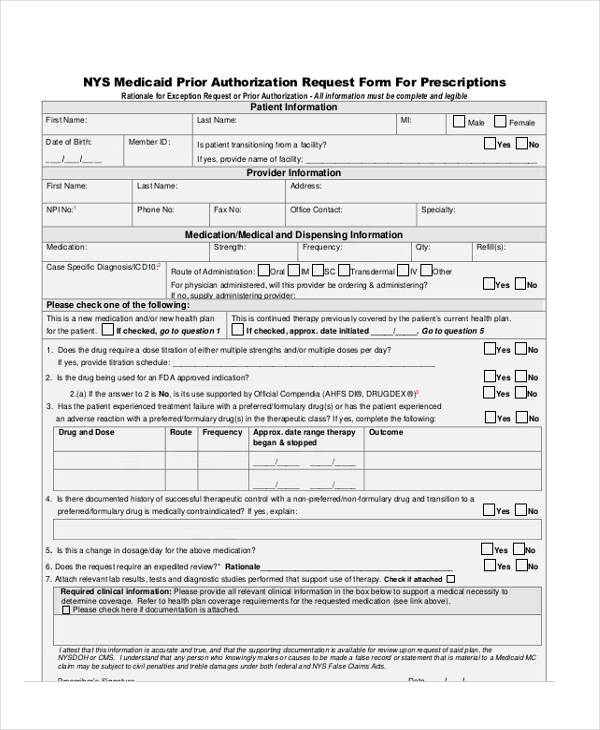
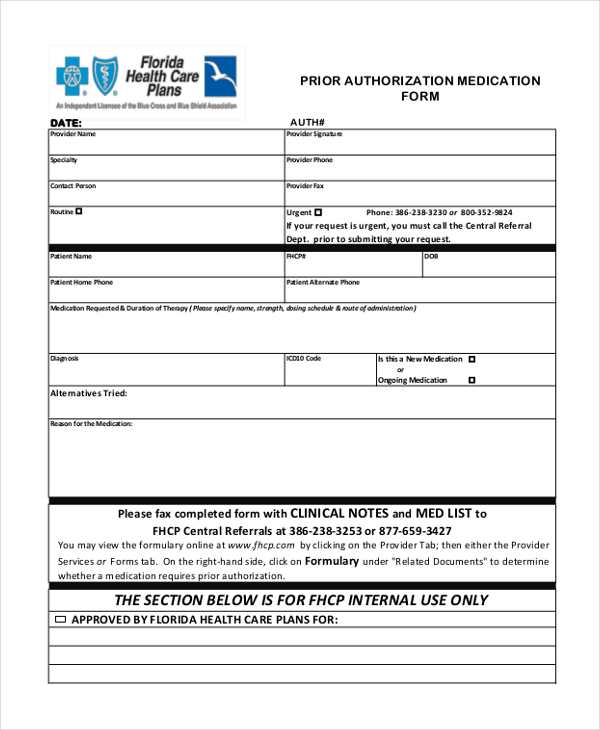
FREE 13+ Prior Authorization Forms in PDF MS Word
Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. For inpatient hospital stays, your doctor will get prior authorization from hap. Emergency room visits don’t require prior authorization. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Prior authorization is a decision by the.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Participating physicians.
Medicare Update Prior Authorization Request Process for Certain
Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. For inpatient hospital stays,.
20152024 HI Standardized Prescription Drug Prior Authorization Form
Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Hap empowered health plan, inc., a michigan medicaid health plan, is a wholly owned subsidiary of health alliance plan of michigan. Approved prior authorizations are contingent upon the eligibility of member at the time of service, timely filing, and claim limitations..
Approved Prior Authorizations Are Contingent Upon The Eligibility Of Member At The Time Of Service, Timely Filing, And Claim Limitations.
Hap caresource™ evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Cms today unveiled a final rule to streamline the prior authorization process and improve the electronic exchange of health. For inpatient hospital stays, your doctor will get prior authorization from hap. Emergency room visits don’t require prior authorization.
Hap Empowered Health Plan, Inc., A Michigan Medicaid Health Plan, Is A Wholly Owned Subsidiary Of Health Alliance Plan Of Michigan.
Participating physicians and providers requesting authorization for medications can complete the appropriate form below and fax to (313) 664. Prior authorization is a decision by the health insurer or plan that a health care service, treatment plan, prescription drug, or durable.