Humana Medicare Tier Exception Form
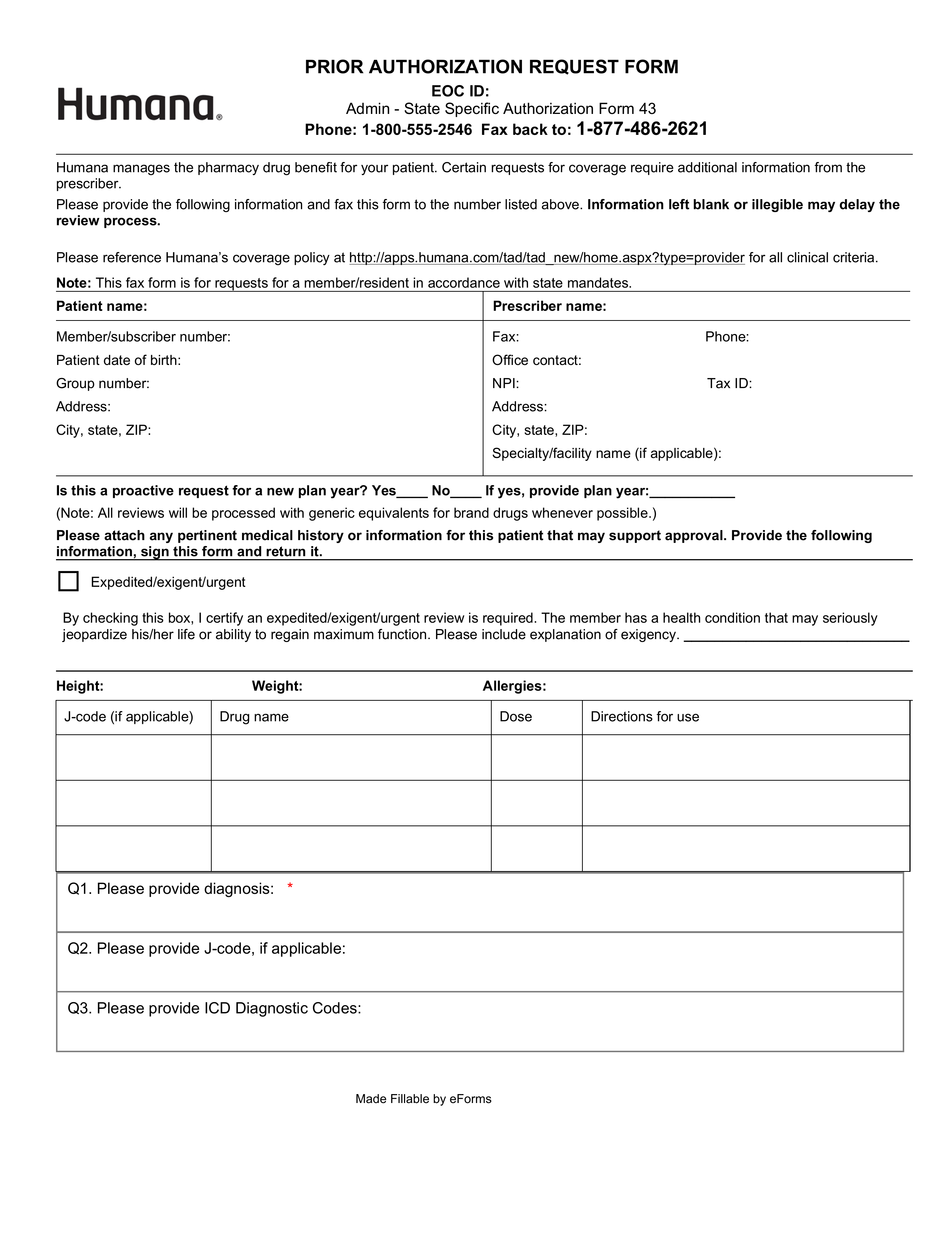
Humana Medicare Tier Exception Form - Humana members can ask for medicare part d coverage redetermination. A tiering exception request is a way to. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Exception requests are granted when we determine that the requested drug is medically necessary for the patient. Find instructions to appeal drug list, coverage rule or. If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. Requests that are subject to prior authorization (or any other utilization management requirement) may require supporting information.
A tiering exception request is a way to. If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Humana members can ask for medicare part d coverage redetermination. Find instructions to appeal drug list, coverage rule or. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. Exception requests are granted when we determine that the requested drug is medically necessary for the patient. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Requests that are subject to prior authorization (or any other utilization management requirement) may require supporting information.
If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Humana members can ask for medicare part d coverage redetermination. A tiering exception request is a way to. Requests that are subject to prior authorization (or any other utilization management requirement) may require supporting information. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Find instructions to appeal drug list, coverage rule or. Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. Exception requests are granted when we determine that the requested drug is medically necessary for the patient.
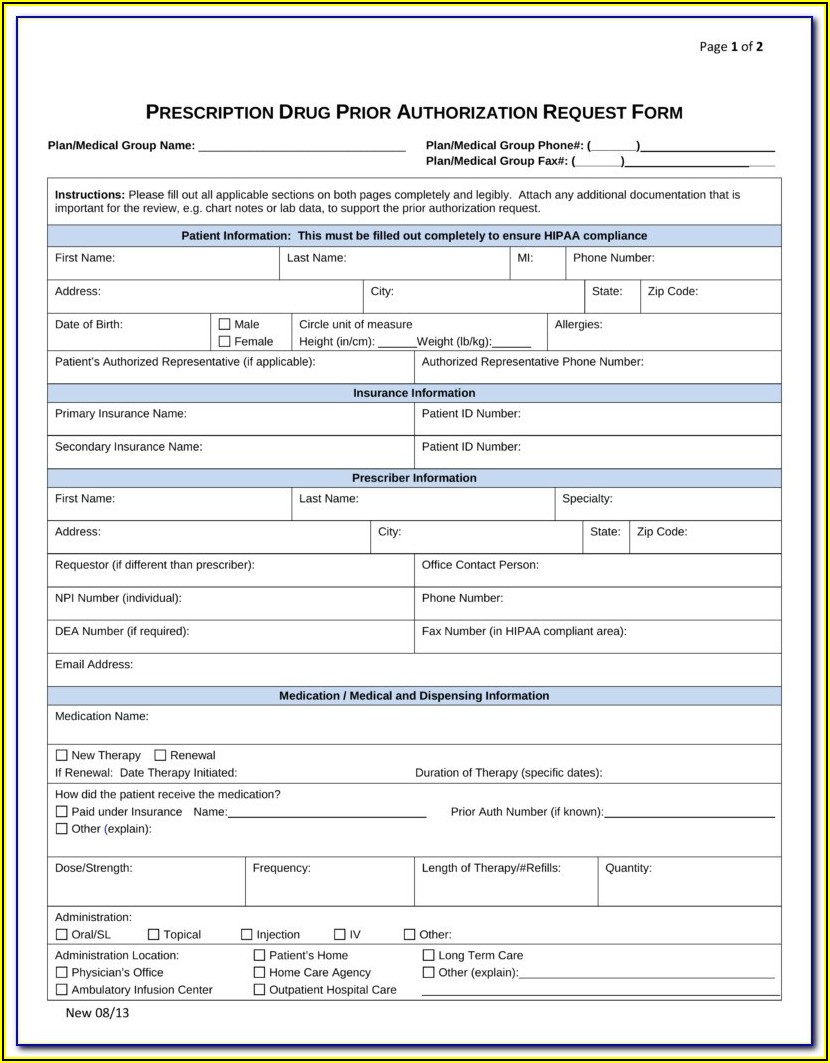
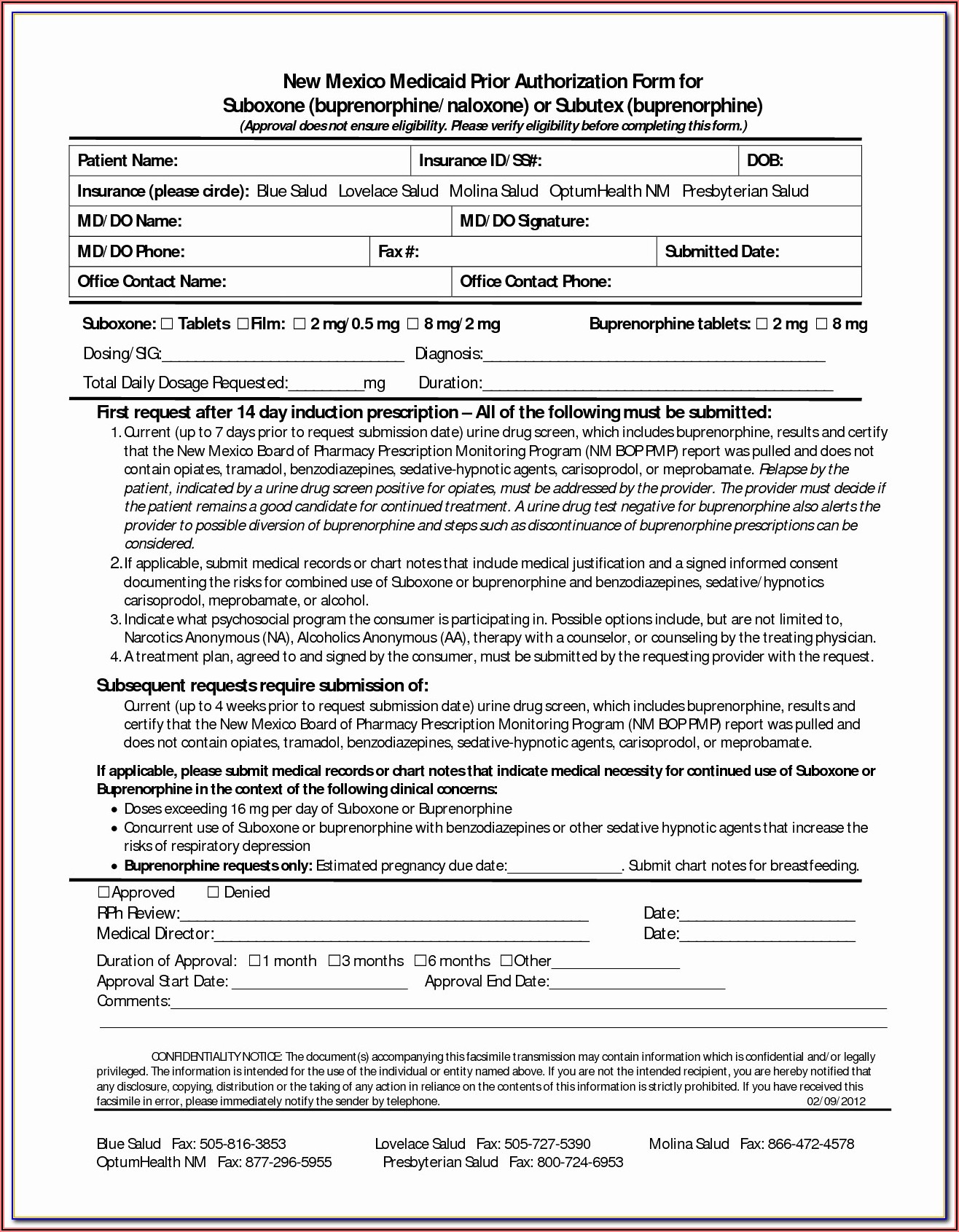
Fillable Online Humana medicare prior authorization form pdf Fax Email
If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Find instructions to appeal drug list, coverage rule or. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Providers should request a tiering exception if they want humana to cover a nonpreferred.
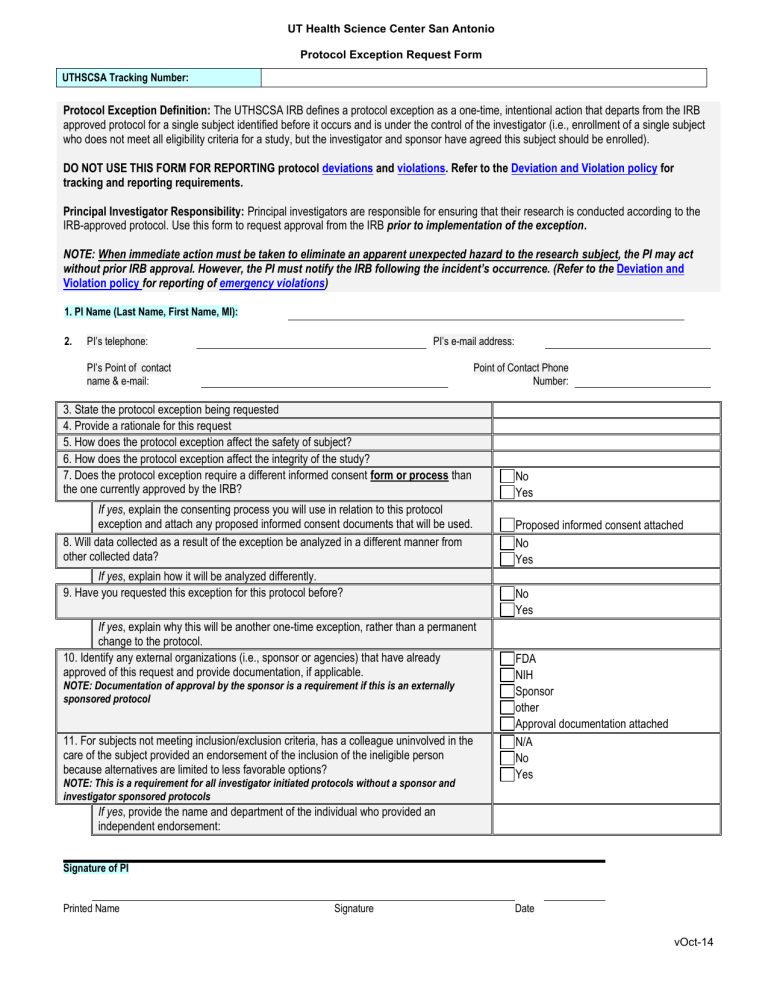
Exception Request Form
Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Exception requests are granted when we.
Fillable Online Humana tier exception request form pdf. Humana tier
Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. Exception requests are granted when we determine that the requested drug is medically necessary for the patient. Humana members can ask for medicare part d coverage redetermination. Requests that are subject to prior authorization (or.
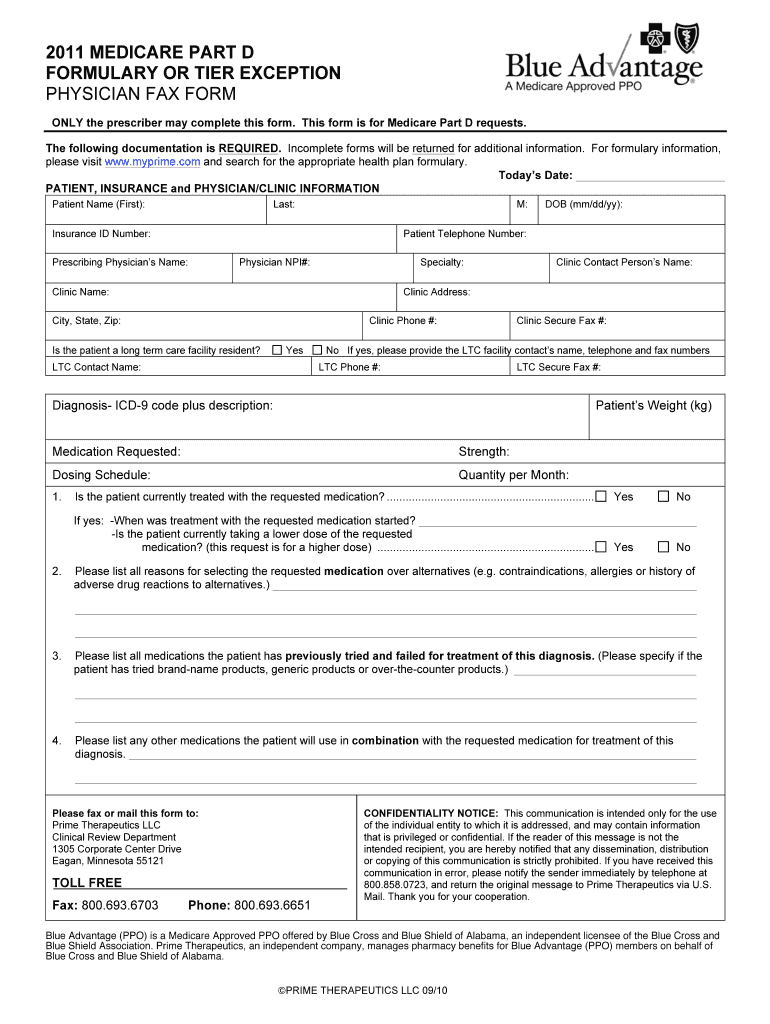
Wellcare Medicare Part D Tier Exception Form Form Resume Examples
A tiering exception request is a way to. Find instructions to appeal drug list, coverage rule or. Humana members can ask for medicare part d coverage redetermination. Requests that are subject to prior authorization (or any other utilization management requirement) may require supporting information. Exception requests are granted when we determine that the requested drug is medically necessary for the.
Medco Health Medicare Part D Prior Auth Form Form Resume Examples
Requests that are subject to prior authorization (or any other utilization management requirement) may require supporting information. If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Exception requests are granted when we determine that the requested drug is medically necessary for the patient. Requests that are subject to prior.
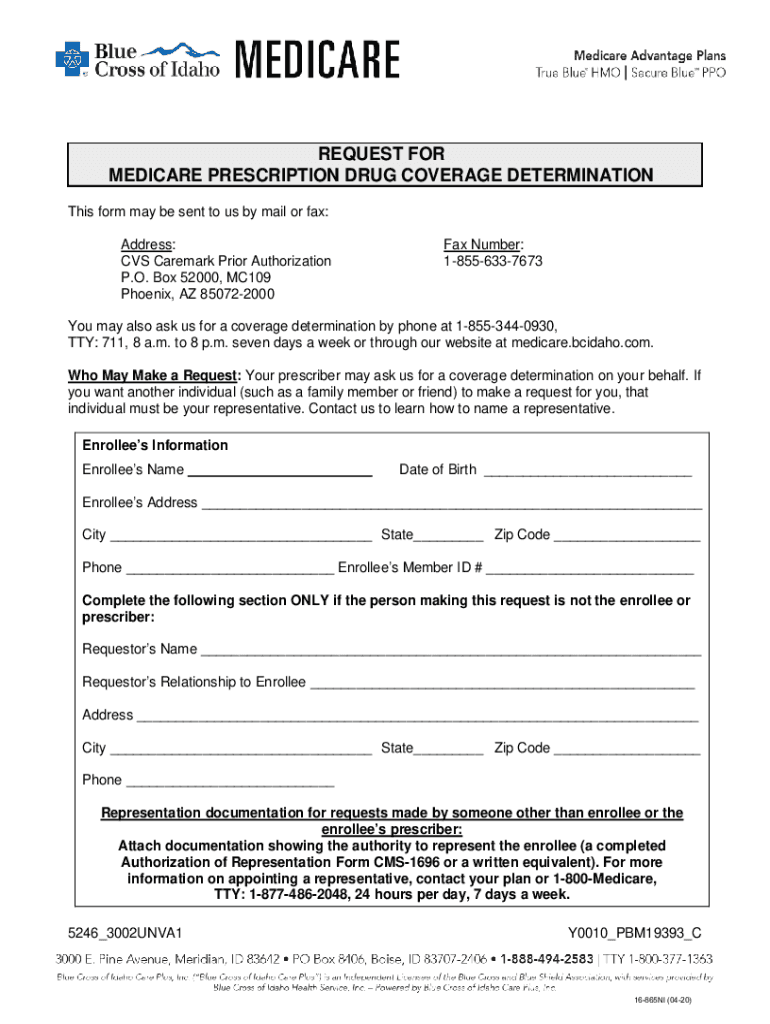
Fillable Online Request For Medicare Prescription Drug Coverage
A tiering exception request is a way to. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Requests that are subject to prior authorization (or any other utilization management requirement) may require.
Tier exception Fill out & sign online DocHub
Humana members can ask for medicare part d coverage redetermination. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Find instructions to appeal drug list, coverage rule or. If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Providers should request a.
Aarp Medicare Part D Tier Exception Form Form Resume Examples
Exception requests are granted when we determine that the requested drug is medically necessary for the patient. If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. Find instructions to appeal drug list, coverage rule or. Requests that are subject to prior authorization (or any other utilization management requirement), may.
Uhc Appeal Form 2023 Printable Forms Free Online
Exception requests are granted when we determine that the requested drug is medically necessary for the patient. Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Requests.
medicare abn form 2019
Exception requests are granted when we determine that the requested drug is medically necessary for the patient. Find instructions to appeal drug list, coverage rule or. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. A tiering exception request is a way to. Humana members can ask for medicare part d coverage.
Find Instructions To Appeal Drug List, Coverage Rule Or.
Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Humana members can ask for medicare part d coverage redetermination. If you cannot afford your copay, you can ask for a tiering exception by using the part d appeal process. A tiering exception request is a way to.
Providers Should Request A Tiering Exception If They Want Humana To Cover A Nonpreferred Drug At The Same Cost Share That Would Apply To Drugs.
Exception requests are granted when we determine that the requested drug is medically necessary for the patient. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Requests that are subject to prior authorization (or any other utilization management requirement) may require supporting information.